Funding for rural and remote health research is at critically low levels, and new research argues for positive discrimination to benefit people living outside major cities.
April’s edition of the Australian Journal of Rural Health reports that an average of only 1.1 per cent of NHMRC funding has gone to health research targeting Australians living in rural and remote areas during the years 2000-2014.
In their paper, Rural and remote health research: Does the investment match the need? Barclay et al estimate the percentage of NHMRC funding at around 2.4 per cent in 2014, an increase from just 1 per cent in 2005.
Each year the NHMRC distributes around $800 million in much needed medical and health research funding. Research topics include better ways of addressing cardiovascular disease, cancer and diabetes, better surgical procedures, valuable epidemiological studies, and better public health initiatives.
Importantly and appropriately, NHMRC prioritises research that helps to improve the health of Aboriginal and Torres Strait Islander peoples.
But, is the benefit afforded by the bulk of NHMRC medical and health research equally available across the country? Do the poor, the ethnically diverse, Aboriginal people, and those living in rural and remote Australia benefit as much as the mainstream?
NHMRC funded research translates into improvements in a whole range of health interventions, but access to these interventions is unevenly distributed across the country.
The short answer appears to be “no”.
NHMRC funded research translates into improvements in a whole range of health interventions, but access to these interventions is unevenly distributed across the country.
For example, access to psychiatrists, psychologists and mental health nurses (and government mental health expenditure) is much poorer in rural and remote Australia than in the major cities (see Figure 1). Any improvement or breakthrough in treating or managing mental illness will be less available for people in rural and remote Australia, simply because there are fewer health professionals to provide that treatment or management.
A similar pattern applies across the board, with the availability of medical specialists, dentists, pharmacists and the full range of allied health professionals in much lesser supply outside major cities. The often-cited maldistribution of general practitioners and nurses is less dramatic than for these other professions, but such comparisons don’t take into account the poorer health and greater need of people living in these areas, and the broader scope of practice of those working there in order to cope with the lack of access to specialist health professionals (such as psychiatrists, psychologists and mental health nurses).
“If a major breakthrough is dependent on communication, technology, a critical mass of patients, on cost and affordability, or on the services of clinicians, then rural people will not be the main beneficiaries,” the article found.
It is hardly surprising that health outcomes outside major cities are worse, with a combination of poorer social determinants (access to work, education, lower incomes, etc), poorer risk factor profile (more smoking, overweight, etc) and lower access to health services.
Research into any of these in relation to rural and remote location has to be a priority. Just about the only area in which rural people score better than those in major cities is that they experience a greater degree of life satisfaction,.
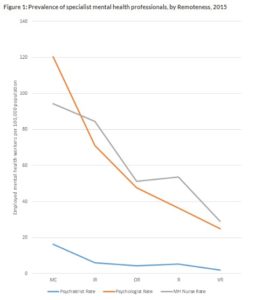
Source: The little book of rural health numbers http://www.ruralhealth.org.au/book/workforce, derived from AIHW’s Mental Health Services Australia.
Barclay et al argue that to address this shortfall, there is a need to prioritise research that seeks to address the imbalance in service delivery or to otherwise benefit the health of people living in rural and remote Australia. This includes a need for research that specifically benefits the 65 per cent of Aboriginal and Torres Strait Islander people who live outside major cities.
“Research is needed to improve rural and remote social determinants and to develop and evaluate services that are fit for purpose and designed in ways that enable optimal clinical supervision and quality control, sometimes in challenging circumstances”.
“The benefits of health research constitute a public good that should flow equitably to all Australians, irrespective of their location,” the authors argue.
It is encouraging to see that the percentage of the funding pool distributed by NHMRC has increased from 1 per cent in 2000 to over 2 per cent in 2014.
But how much should it be?
Clearly, there is some degree of access to the fruits of medical research even for those living in the most remote locations.
But until the level of access to services, and the health profile of people living in these areas reaches that of major cities, the NHMRC needs to commit a greater level of research funding to rural and remote health priorities.
“The benefits of health research constitute a public good that should flow equitably to all Australians, irrespective of their location,” the authors argue.
“With research assets, as with infrastructure and clinical services, some positive discrimination is needed to balance the natural challenges of space, time and place.”
Photo by Cristina Gottardi on Unsplash
