Photo by Henrique Félix on Unsplash
I am passionate about improving health outcomes for young people in rural, remote, and regional (RRR) areas in the Northern Territory. As a first-generation Indian Australian, growing up in a regional town in the Territory was challenging. I faced many obstacles making it difficult to reach out for help. Although I was lucky enough to have support mechanisms encouraging me to seek help, I understand that it is not the same for everyone. This is especially true for young people from culturally and linguistically diverse backgrounds. There is a huge stigma around seeking mental health assistance. However, if you are facing mental health challenges, you must reach out for help.
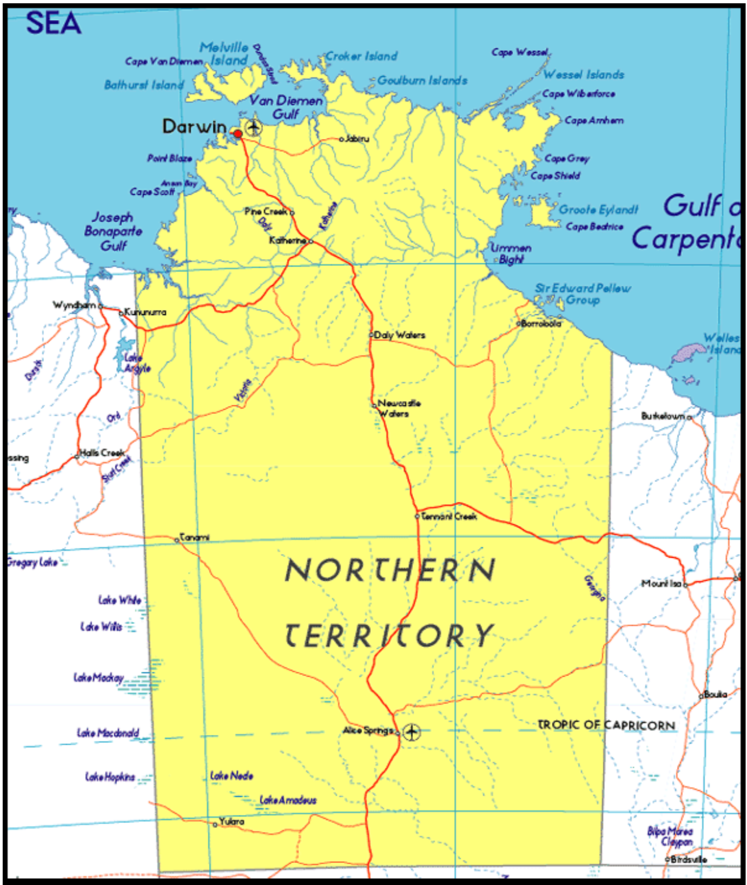
It is a sad reality that young people in RRR areas have difficulty accessing health care facilities. There is a lack of health services and mental health education for RRR youth compared to urban counterparts. RRR regions of the Northern Territory have been underrepresented in the conversations regarding health and wellbeing. It is high time for our voices to be included in nationwide discussions since our challenges are far different from the rest of Australia. There is a need for local solutions to local problems to ensure equity in health services.
Mental health and related issues are the biggest concerns affecting young people in the NT. About 16.3% of the issues impacting residents are related to mental health and substance use disorders in the NT. This is compared with 7.4% nationally despite only consisting of 1% of the Australian population. Alarmingly, NT has the highest rate of child death due to suicide. Apart from the scarcity of services, there is a lack of resources responding to these challenges in a culturally appropriate and specialised manner.
… the only choice is a three-hour drive to Darwin to access a bulk billing practice…
For anyone, the first point of contact for individual mental health concerns is their local General Practitioners. However, there are no bulk billing services available in Katherine (a regional town 320 km southeast of Darwin). And, while you can claim for the Medicare rebate, a lack of bulk billing services limits low-income Territorians in RRR areas from accessing health care facilities. For people not able to afford GP fees and not eligible to access the Aboriginal Community Control Health Organisations, the only choice is a three-hour drive to Darwin to access a bulk billing practice. The next available bulk billing service for people living in Tennant Creek (a regional town 1000 km south of Darwin) is a 5-hour drive to Alice Springs. It would be great to have a mental health care travel cover plan specifically for RRR residents, where financial support is provided for travel and consultation expenses.
The Northern Territory Mental Health Strategic Plan (NTMHSP) 2019-2025 was established to enhance the mental health and wellbeing of Territorians. In NTMHSP, Priority Area 5 is evidence-based research. To deliver quality services, both the Territory and Federal Government must acknowledge the diversity of the NT and understand the ‘one size fit all’ method won’t work here. The health concerns and service deficits of the Katherine region might be different to the Barkley region or Darwin. There needs to be federally-funded region-specific research to understand what the community needs and make tailored arrangements. This region-specific research should be in the form of consumer consultations with the involvement of research institutes and the NT Department of Health. Additionally, the research should be codesigned by community members with lived experience along with specialists to ensure research impact and good outcomes for local communities.
The Summit is driven by young people discussing topics such as mental health…
While being critical of the current deficit of the system, it is essential to acknowledge great initiatives and improvements happening in the Territory, such as the incorporation of youth voices in decision making and policy. The Menzies Youth Health Summit was held this year and previously in 2019. The Summit is conducted by the Menzies School of Health Summit in partnership with the Government, and non-government bodies. The Summit is driven by young people discussing topics such as mental health, sexual health, inequities in services and even climate crisis. A report is developed every year after the Summit by researchers, and decision makers should incorporate outcomes of the Summit into their practice.
Prevention is better than cure
Priority Area, 4 of NTMHSP 2019-2025, focuses on improving the mental health literacy of Territorians and investing in different mechanisms to close the gap for individuals living in RRR areas accessing services. Currently, there is no NT-specific funding for mental health education directly to high school students, who are most at risk of mental health issues. Although, there are organisations providing free Mental Health First Aid (MHFA) for young people. These projects are funded through NT Government grants. There is a potential to make it mandatory for all young people to participate in free MHFA training delivered in high schools across the NT, in schools or elsewhere. Research has shown that MHFA training will helps to improve the knowledge and beliefs of the participant in relation to their capacity to recognise or prevent worsening mental health. Moreover, MHFA training can increase mental health literacy in the community and aid in reducing or overcoming stigma.
Poor health literacy is not just a Territory issue, it is an Australian issue. There are excellent free resources for young people, but there is a lack of knowledge about existing services. With time I hope, we can have louder conversations about destigmatising mental health issues and ensuring adequate access to resources available to people in RRR areas. If the barriers in seeking early interventions are abolished, communities can foster healthier practices in seeking assistance before it becomes too late to save a life. This is a contributing factor to the current burden of disease in Australia. There are multiple factors regarding social and economic disadvantage that contribute
te to poor health literacy in RRR areas. But, with government support, we can start addressing some of these barriers earlier, leading to better outcomes for all. More young people from NT are stepping up to share their mental health struggles and calling for adequate mental health services.
About the author
 Alina Biju (she/her) is a Bachelor of Science (Biomedical Science) student at Charles Darwin University from Northern Territory. She is deeply interested in health research, public health, and youth engagement. She is also a member of the 2021 NT Youth Round Table, and an NT representative on the Australian Youth Affairs Coalition Young Leaders and Advocates Fellowship. Alina believes that if young people are equipped with the knowledge to make healthier life choices, they will have better public health outcomes
Alina Biju (she/her) is a Bachelor of Science (Biomedical Science) student at Charles Darwin University from Northern Territory. She is deeply interested in health research, public health, and youth engagement. She is also a member of the 2021 NT Youth Round Table, and an NT representative on the Australian Youth Affairs Coalition Young Leaders and Advocates Fellowship. Alina believes that if young people are equipped with the knowledge to make healthier life choices, they will have better public health outcomes
